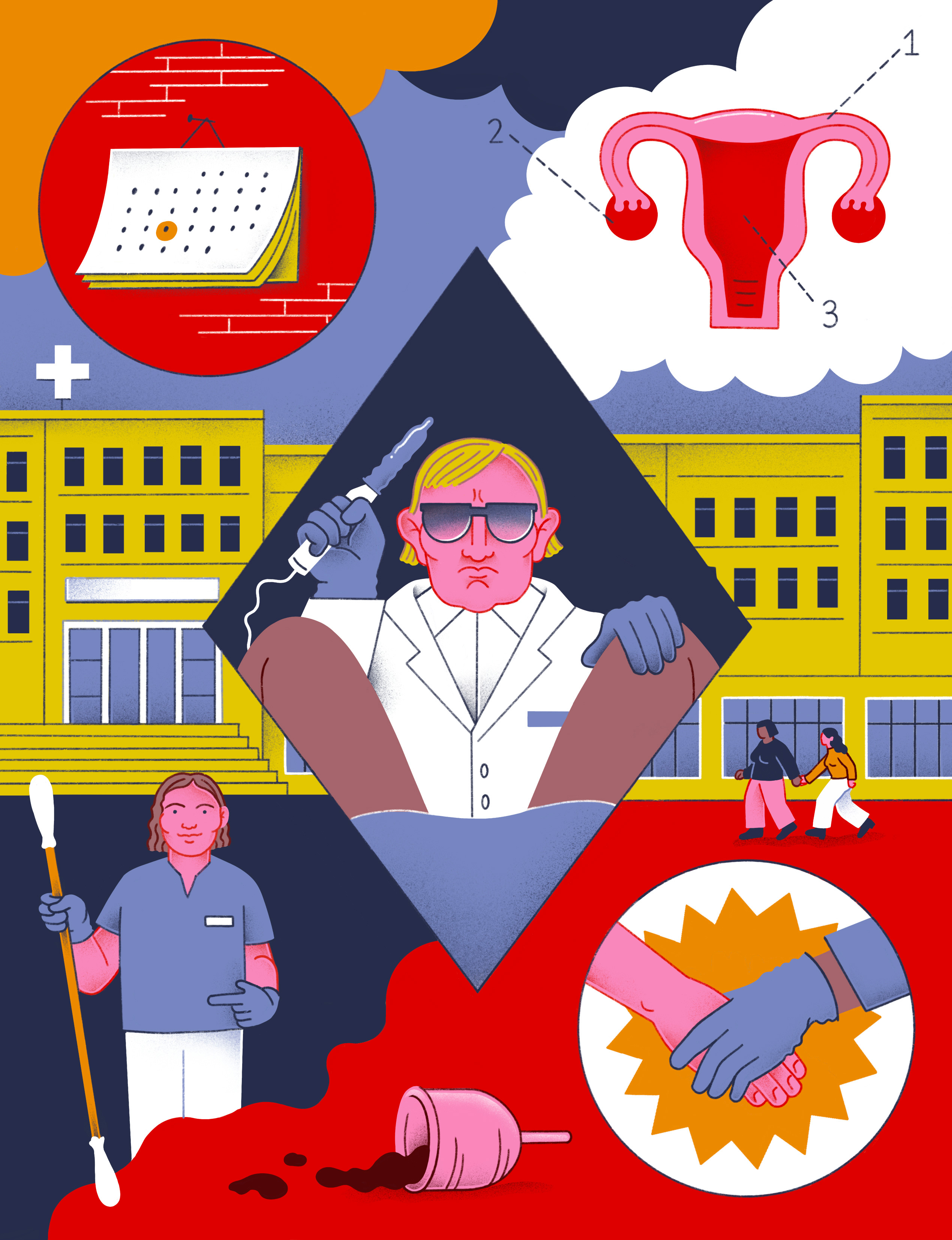
Multiple obstacles to going to the gynecologist
- The first contact of several young people with the gynecologist is usually complicated. Aroa Sotelo (Bilbao, 1998), Ainhoa Labairu (Bilbao, 1998), Naiara Martín (Mar del Plata, Argentina, 1990) and Uxue Rey (Pamplona, 1997) tell us about their experiences and concerns. They stress the need to attend earlier and denounce the coldness of medical men. They criticize the fact that there is a complete responsibility to serve users.
Young people who travel down the street are chatting around the gynecologist. You're called to go to the office and you seem worried, surprised and a little scared. “Have you gone?” she asks them nervously. One of them answers yes and asks: “When was it? How was that? What did they do? Does it hurt?” Everyone starts sharing experiences.
A short time ago Aroa Sotelo asked for the first gynecologist appointment to do the exam. She went to the medical family, but had difficulty taking the time: “He said: "But are you right? '. I told him I've never gone, it's time to do the test." The doctor responded that he needed a “weight reason.” However, he offered help in making an appointment: “He saw that I was little in the history pain by the rule and asked if I had pain now. I told him yes, he told me that by that route I can get the appointment.”
Sotelo thanks the doctor for his help: “I think it has influenced the fact that the doctor is a woman.” He denounces that the health system does not address the gynecological issue: “They don’t give importance to our health and our problems, and it seems that something must happen to us.” As he requested the appointment in Easter and the doctor was on vacation, he had difficulties: “They didn’t put substitutes, that means there are no people listening to us. It seems that we have to be dying from pain to be cared for.”
Going to the gynecologist is afraid of Sotelo: “It is unknown and the procedure can be very invasive”
He hasn't gone to the gynecologist before because he's scared: “It is unknown and the procedure can be very invasive.” In addition, he considers that the experience can be very different according to the gynecologist: “I hope she’s a woman. There are certainly professional men, but I'm afraid to feel embarrassed or forced." Although it is necessary for health, he says it is “very intimate”.
It would be “easier” to go to the gynecologist’s office if she had more training and information: “If we were to speak from a young age, we would have less shame.” He denounces that the eyes are seen from the cysheterogenic: “Although not true, they assume that I am a woman and that my partner is a man and therefore we use the condom.”
Gynaecological violence
Ainhoa Labairu first came to the gynecologist at age 16. He denounces that the doctor committed abuse and that it was “very aggressive”. So you don't want to come back: “It gives me a lot of trouble and anguish.” The experience was hard, so you don't really want to enroll.
Despite being an irregular month from time to time, he went with his mother to the medical family because a summer was “constantly” bleeding. They worried and sent him to the gynecologist. In the consultation there were two people: a “serious” old man with glasses, gynecologist, and a woman about 40 years old, nurse. They didn't explain what they were going to do. “I saw that they had pulled out a kind of silver stick, quite long, and that the gynecologist had told the nurse to pass the other one, which seemed bigger. Without notifying me, it was terrible.” More than pain, he says he felt “discomfort” and “surprise.”
Then, without saying anything, the doctor put his hand in the vagina: “I remember that I had one hand inside and another outside and started beating on the uterus. I felt enormous pain and discomfort.” When he was lying down, the nurse would shake his hand and give him some reassurance trying to help him: “I felt sorry, I said: ‘Quiet, does it hurt?’ He denounces that the man was by his side: “The nurse was taking care of me and touching the guy, without saying anything, what he wanted.”
Labairu says the context was “very cold” and “rigid”: “I had before an aseptic man who did not express any point of emotion”
She told her that she had irregular months and recited hormonal contraceptives: “I think he sent them to me because I couldn’t see anything. When we left the room my mother told me that she would not take them and broke the prescription.”
Labairu believes that the experience could be different if the mother was next to her and explaining the procedure: “I was 16 years old and didn’t know what they were going to do to me. He also raised his hand and sat next to him, as if nothing had happened.” He clearly saw the “totally rigid” image of masculinity: “Why does the nurse have to show her willingness and care to help, and cannot the gynecologist offer it?”
He adds that the context was “very cold” and “rigid”: “I had before an aseptic man who did not express any point of emotion.” That is why I fear to return: “I know I would act differently, but I would be afraid to think about who would touch me.”
Barriers to appointment
Naiara Martin first goes to the gynecologist this year. She doesn't really want to enroll because she's a trans woman and she fears transphobia. He operated in Thailand because in Navarra there is a 10-year waiting list. The surgeon told him it was necessary to follow up to make sure everything is okay. “I came with a letter that made it clear that a gynecologist had to take care of me.”
He went to the transaction to request an appointment at the transgender and intersex care service in Navarra: “I was told that I didn’t need a gynecologist, because when we see signs of uterine cancer or people go only for checkups.” Despite showing the letter, he was told that he first had to talk to the endocrine and that he told him who was going to attend: urologist, gynecologist or plastic surgeon.
Meanwhile, he went to the Estella Health Center and immediately placed on a waiting list. They called a month. She stresses that the attention was “reasonable”, “honest” and “close”: “They had no experience with women who undergo such interventions, but they did with cis women and boys.” First of all, he explained what he was going to do, and as everything was fine he told him to come back in three months: “He told me that if I had any problems, he would call me back.”
Martin believes he is a “lucky” because he has quickly linked his quote: “A friend who lives in Bilbao has a wound in the vagina and is cited in five months”
Before going to the doctor, the concern about the transfobe positions was that it felt “very good”: “I thought that the people could have a more closed mentality and that I could feel rejected, but now I know I could come back.”
In Transbide he was sent to the endocrine: “As I wasn’t a gynecologist, I put on gloves and looked at me a little from the outside.” Then, they didn't call for gynecologists. Although Transbide has a specialist gynecologist, he was told he could not attend because he is about to retire: “It is not my responsibility that there are no gynecologists, they have to ensure that a person takes care of us.”
She's happy because she's got a referral gynecologist through her medical family. However, he believes it is a “lucky” because it is rare to associate a quote: “A friend who lives in Bilbao has a wound in the vagina and is cited in five months.” Martin has also denounced that users are responsible for treating it: “We have to be able to get the care we need.”
Need for ‘weight reasons’
Uxue Rey joins the insistence on asking: “We seem to have to ask the amateurs for tests. I don’t know how many times it’s best to do it, but unless someone asks for it, they don’t feel they’re asking for more than they should.” He thinks that can make him go less.
Rey, a private and public gynecologist, describes two first times. At 14 years of age one: “A relative suffered a serious gynecological problem about 40 years ago because it was not detected in time. As I was afraid to be myself, he took me to a trusted doctor.” He was attended by a private gynecologist: “Not because we are not at all suspicious of the public, but because in this case the relative wanted to address that person.” He has a rather “diffuse” day, but believes that they did not give him many explanations: “And if you give me, I didn’t understand them.” They asked him if he had sex to do the test in one way or another. The visit was “strange”: “I was a very mature man, imagine, I remember the colors of the tie.”
Rey denounces the existence of a “great lack of control”: “Assistance to the gynecologist is in the hands of his decision”
Six years later he thought it was time to do a study. “My mother encouraged me because I knew I already had sex with other people.” She talked to the family doctor, but they only gave her the time with the nurse: “Why do you want?” the doctor asked. And I told her I wanted to do the test. "But something happens to you? ', he told me. What is having something? A pain? Any concerns?”
Finally, he recently performed the first cytology at the Navarro Center for Sexual and Reproductive Health Care in Andraiz: “It’s a place of reference for me.” Rey’s addicts have not yet done cytology and believe that it is “by chance”: “When two months were short to turn 25, I went to the gynecologist because I had pain. As I was there, they told me they were going to do everything.”
He denounces the “great lack of control”: “Assistance to the gynecologist is in the hands of his decision”. Although he believes it is necessary to go before, he emphasizes that “the ideal” is not going private: “The public health system should ensure care.”

Preventive cytology for those over 25 years of age
Why is cytology performed at age 25? Why not before? What tests can be ordered? Gynecologist Marta Ruiz and nurse Itziar Ayensa answered these questions. They both work in Andraiz.
Cytology aims to prevent, detect infections or pathologies associated with cervical cancer. That is, it is not about detecting people who already have cancer, but those who have no symptoms, but who may have some predictable injury and who over time are at risk for uterine cancer.
Cervical pathology is related to human papillomavirus, sexually transmitted infection. That's why they only do cytology with people who have sex with other people. Ruiz has explained that the incidence of uterine cancer under 25 years is “very rare”.
According to Ruiz, cytological alterations or “small” and transient alterations are frequently detected by cytology: “Among young girls the incidence of HPV infections is quite high, but their immune system responds better and the rate of HPV elimination is much higher.”
Warns that doing so may be harmful before: “It can lead to high economic costs, unnecessary treatment, weakening of the immune system and psychological effects.”
Ayensa works on the development of cultures for the detection of cytology and infections in nursing: “If there are problems we send them to the gynecologist.” Before performing any tests they explain everything: “We’re slowly explaining every step we take, such as telling them we’re going to put the speculum in and it’s not painful.” The goal is for patients to be “quiet” and not unpleasant: “By position it will always be a little unpleasant, but we will try to make it as enjoyable as possible.”
In Navarra there is no automatic screening for people with utero, that is, they are not called when they are 25 years old. Therefore, Ruiz comments that there are two ways to ask for the observation: “Observation is opportunistic, that is, we only call those who have come for other reasons, because they are already in the system. Another option is to call them and ask for the time.” Therefore, in the case of those who have never been in the gynecologist, they place the responsibility of calling them. However, in Navarra the system is being modified and a population screening is being carried out, for the moment for those over 25 years. In the rest of the Basque Country it is also being tested in the public system for those over 25 years.
In addition to cytology, other reviews are made in Andraiz. Ruiz has emphasized that the Sexual and Reproductive Health Care Centers are open to any question or concern: “If you haven’t turned 25, in principle everyone is available for health education, sex education, sexuality, any issues related to sexually transmitted infections and the issue of contraceptives.”
She points out that there are also educators and that their work is very important: “There is no waiting list and you can go with anyone, like friends, alone or as a couple.” It invites young people to visit the Sexual and Reproductive Health Care Centers.