The myth of osteoporosis
- Gillian Sanson is a women's health educator. He currently resides in Auckland, New Zealand, where he has worked in the Family Planning Society. The Osteoporosis ‘Epidemic’: Well Women and the Marketing of Fear and The Myth of Osteoporosis are the best known books in the world. Here we have translated the essence of Sanson's short article in the publication of the Canadian Women's Health Network.
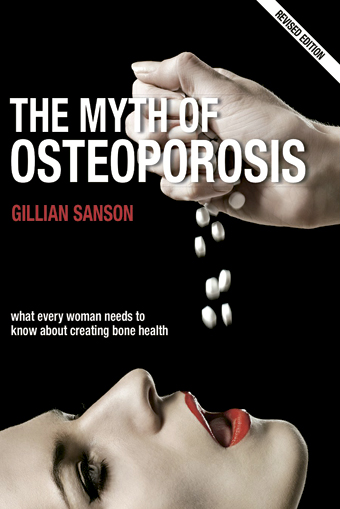
Millions of people are driven to check for osteoporosis and, to avoid it, to take the medication the alarming statistics of bone fractures, aggressive advertising and smart doctors. We are told that the tests are appropriate and that the drugs they offer us are safe and effective, but we must give them a more critical look.
Statistics, of course, cause astonishment. The Canadian Osteoporosis Association estimates that one quarter of women aged 50 (25%) and one in eight men have osteoporosis. The Osteoporosis Foundation EE.UU. points out that half of the population over 50 years of age has suffered some osteoporosis fracture and that at least 34 million people suffer from osteoporosis, a history of osteoporosis (low bone density), and that 20% of hip fractures die in a subsequent year. However, in contrast to the above data, the Mayo Clinic highlights that 21% of women who have overcome menopause suffer from osteoporosis and 16% suffer from some rupture.
Until the level of low bone density was determined in 1994, osteoporosis was not common, it was called a disease that affected the weak bones of very old people. With age, we all lose bone density, but the new definition doesn't take it into account. It takes a young woman's bones as a reference standard, making it impossible for an older person to have a normal diagnosis. The check-up turns what is nothing but a risk factor into a disease, but it does not clarify anything about the hardness, architecture, organization, size or appearance that have to do with bone weakness.
Although academic institutions in Canada, the United States, Sweden, Australia and the United Kingdom state in their research that densitometry does not adequately identify which person will suffer a bone fracture, the new definition of osteoporosis remains dominant. It should be noted that a study conducted by the University of Leeds has shown that people with higher bone density have suffered 63% of fractures. All bones can break if they are forced to do so. Higher or lower density has so little importance that it is not worth measuring.
Most people under the age of 80 have no symptoms and do not realize that they have osteoporosis. 12% of women aged between 50 and 79 suffer from spinal compression (vertebral rupture), although most do not even realize it. It is a small percentage that has symptoms and most get well. As Dr. Bruce Ettinger, a specialist in osteoporosis in California, says, “osteoporosis that causes pain and incompetence is a very rare disease.”
The hip fracture that occurs in older people is not due to low bone density, but to small household risks, immobility, dementia, medications such as corticosteroids, the coincidence of many drugs, lack of vitamin D or diseases such as hyperthyroidism, crohn's or celiac. In other words, the greater the person, or the worse the person is, the greater the risk that a bone will fall and break.
Television commercials, journal articles and papelites from medical consultations reveal the importance of osteoporosis in our lives. Experts also agree on this.
With the new definition given in 1994, the giant trailer “to prevent osteoporosis”, which includes the pharmacy industries, check bone density, dairy and calcium. Some medicines that say “prevent” osteoporosis, especially bisphosphonates, Fosamax and Actonel, have been available for a decade and have been increasingly famous for the decline in hormone therapy recommended for decades for menopause. But have you properly tested these new medicines in terms of their safety and effectiveness?
Sales of bisphosphonates have increased worldwide to unseen figures. Fosamax’s sales have risen from $1 billion in 2000 to $2.7 billion in 2003. In the meantime, we still do not fully understand the mechanisms of the effects of bisphosphonates, and many experts warn that we need to learn how to prescribe them carefully, to better understand in the long term the effect that medicines have on preventing or slowing down bone restoration. In fact, although with the drug it can become denser or more mineral-rich bone, there is concern that if this bone is not reconstructed, it will become more fragile and more prone to small fractures. Animal research has shown that this is the case. Bisphosphonates have a long-term effect and it is known that they stay in the body for more than 10 years, influencing both good and evil. It is unethical to use this medicine in pregnant women or in women who still have bisphosphonate in their bones, which may be pregnant.
Bisphosphonates can suffer very serious collateral damage to the apparatus and annoying consumption. For all these reasons, the performance they offer is insignificant or very low. Fosamax can reduce hip fractures by 1% (and this is also being discussed). This means that 80 women at risk must be treated for three years to prevent one of them from breaking in the hip, while another 79 will have no benefit. It is estimated that hundreds of 50-year-old women with weak bone density should be treated for three years to prevent a hip fracture in each of these groups.
Recently, a study shows a new complication of bisphosphonate therapy: dentists have found osteonecrosis (dead bone) in receptor mandibles. Ego Seeman, an important specialist in osteoporosis, has warned: “Have we not yet answered the question of whether these medicines reduce or increase the risk of long-term bone fracture?”
Uncalculated risks may also occur after acceptance of the medicinal product, as demonstrated above by the serious risks associated with hormone therapy.
In these times osteoporosis is not called “women’s disease”. But it works like a fever to offer expensive and dangerous medical solutions to the fragile bone density of healthy men and women who have never suffered from the disease, so we look away at the really serious problems: avoiding the falls of the elderly and diagnosing the real sick.
BRN + Neighborhood and Sain Mountain + Odei + Monsieur le crepe and Muxker
What: The harvest party.
When: May 2nd.
In which: In the Bilborock Room.
---------------------------------------------------------
The seeds sown need water, light and time to germinate. Nature has... [+]