
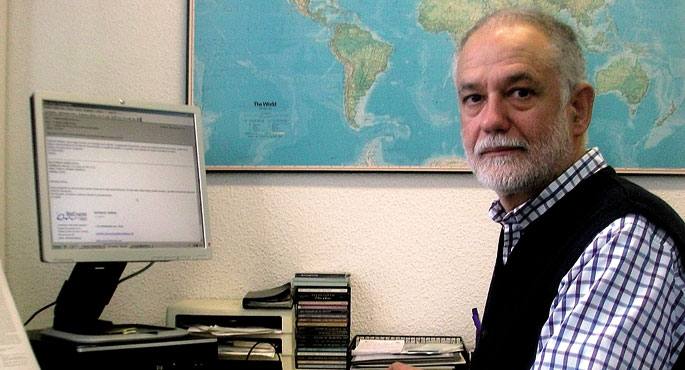
- The pilot experience Make Healthy Life has been two years in four centers in Osakidetza. Prevention is fundamental in health, we can avoid 50% of deaths by changing life habits, but how do we get the population to adopt healthy habits? We asked Gontzal Grande, head of research at the Primary Care Center in Bizkaia, responsible for the initiative.
Why is it important to promote a healthy lifestyle?
Today we know, according to all the studies, that the main diseases that deteriorate or kill us are largely the cause of life habits. Inadequate food, physical inactivity, and tobacco and alcohol use are responsible for nearly 20,000 deaths annually in CAV, some 10,000 of them. By performing half an hour of daily physical activity, eating in a balanced way, not smoking and drinking to measure, we would avoid 50% of the deaths and 80% of the most common chronic diseases (heart attacks, cardiovascular system, diabetes, cancer…). These are incredible numbers, there's nothing that has that potential impact.
But we don't know how to get citizens to adopt healthy lifestyles, because we're socially losing that struggle. It is true that on the subject of tobacco things are changing and burning less and less, but we are losing the fight in other habits (diet and physical activity) and are the factors that have the most impact at the moment. For example, the lifestyle that is being imposed in the last 50 years has been a sedentary lifestyle (we drive everywhere), a higher proportion of obesity among children and young people… In addition to the wills and values of our own, we also perceive the influence of society and the environment. One way to deal with all this is to adopt measures in the network of primary care services that we have in the neighborhoods and towns, as we are doing with this program, but it is necessary to act from different areas. This is not only the responsibility of the health sector, we have collaborated with the educational agents of the neighborhoods that we have launched the program, with the work centers, with the city council, with the sports club, with the associations of the neighborhood … to agree on messages and criteria.
From a clinical point of view, what is the procedure followed by the program?
The first step has been to make health workers aware of the importance of life habits. We are all aware, but when you dig a little deeper and realize how much lifestyle influences disease, professionals are aware of the priority of correctly conveying the message to citizens. Patients are often informed of tobacco or alcohol, but about 70% of the citizens who have participated tell us that they have never received messages about the diet or physical exercise that suits them with doctors or nurses. Moreover, sometimes they receive contradictory messages and those who have a heart problem may leave the appointment thinking that it is not convenient for them to exercise.
Having become aware, based on common bases and criteria, the center itself has organized the dynamics of starting the program: how to obtain information about the habits of the approaching citizenship, how to give recommendations based on them, how to help plan changes in habits… And with the significant evolutions that occur in all these tasks, from the research center we send them a report every month to reflect and continue improving the strategy.
In practice, what kind of recommendations do they give?
Where applicable. The Primary Care Service develops a permanent relationship with citizenship, the physician has a great knowledge of his/her health status and can adapt his/her advice accordingly. We have provided imaging material to doctors to facilitate the sending of the message and, for example, to make those with asthma aware of the benefits to the respiratory system of smoking cessation, physical activity, etc. Since these habits affect all body organs and systems (cardiovascular, respiratory, endocrine, neurological…), connections can always be established between them according to the state of health of the citizen. Standard advice, such as “you have to exercise,” serves little, and it’s more effective to help you develop a plan, agree on realistic, step-by-step goals. As if it were a drug, but reciting diet, physical exercise or measures to stop smoking.
In addition, recommendations have been given to people who, as a prevention programme, do not suffer from any disease. Health centers spend almost the entire population and we should take advantage of this visit, although it has approached the usual analysis, to talk about the importance of these habits, whether they are sick or not, regardless of their age.
You mentioned four main factors. Are you aware of something else?
We currently know the ranking of risk factors, the most dangerous factors for the incidence of diseases, and we have set the priorities accordingly. Diet, physical activity and tobacco are the top of the ranking, then there is alcohol abuse and we also take into account biological factors (hypertension, hyperglycemia, obesity…), environmental pollution or consumption of other drugs. But according to the most prestigious studies, both in death and in the loss of quality of life, the influence of food and physical activity is fundamental. In addition, as a physician, it is easier to influence these factors than environmental pollution.
At what level is prevention important for the survival and maintenance of the health system itself?
We have a demographic and epidemiological description that the health system cannot maintain. The control of communicable diseases and the improvement of quality of life have contributed to raising life expectancy in recent years, but at the same time, as we get older, we accumulate many chronic diseases, which requires a lot of medical treatment. Chronic diseases consume 80% of the economic budgets. With the lengthening of life expectancy, we must ensure that there are no diseases in that life and we know the formula: if we do a physical exercise of at least half an hour a day – we are not asking for a huge effort – if we take a diet rich in fruits, vegetables and fish, we stop eating too many meats, salt and polysated fats; and if we avoid tobacco we get to age 100 and in many of those years we will not have diseases. In economic terms, prevention should also be a priority issue, but most of the money goes to care. It is illogical, for example, to allocate the budget to care for those with diabetes, when in adult diabetes more than 90% of the supply is food and physical exercise.
To what extent do we make our health available to doctors and delegate our responsibility to our health?
In particular, the program goes against the medicalization of health, because it reminds the citizen that health depends above all on oneself, on his way of life and on his habits. We emphasize the responsibility and care of oneself, whether due to illness or not, as these habits will mark the future, and we can help you along that path. The environment also has to do with, of course, exogenous economic, social, cultural factors and it is not the same to live in a town full of bidegorris as in a city designed for cars, but the choice of one is fundamental. People have to be educated, starting with school, but also throughout their lives, and it is not a bad thing for the doctor to occasionally go through health prevention measures. People no longer know whether eating eggs is good or bad, there is a lot of misinformation, and the doctor is responsible for updating them and transmitting the information correctly, to inform the citizen that physical exercise and being an active woman is much more effective than an early breast cancer screening program.
How many people have participated in the programme, what results have you achieved and what future has the initiative now?
For two years now, we have four villages in operation: In Sondika, Matiena, Bilbao La Vieja and Beasain we have worked with about 80,000 inhabitants. Compared to citizens who have not participated in the programme, an additional 6% have managed to change their living habits thanks to the initiative. But it is a pilot test and the most important thing is that, thanks to the obstacles and strategies learned in the centres in Osakidetza, we are ready to extend the initiative to the centres in Osakidetza that want to participate more effectively. The implementation will be carried out in dozens of centers, as it is an important change and the will of the centers is fundamental: this action alters the structure of the centers, since the centers are currently focused on disease care, not prevention. We cannot enter overnight in the 319 centres that have Osakidetza.